

|
|
DR. EMAD AZIZ, D.O., MB.CHB, FACC AMONG FIRST IN THE UNITED STATES TO IMPLANT NEW DEVICES TO TREAT A SLOW HEARTBEAT |
|
|
|
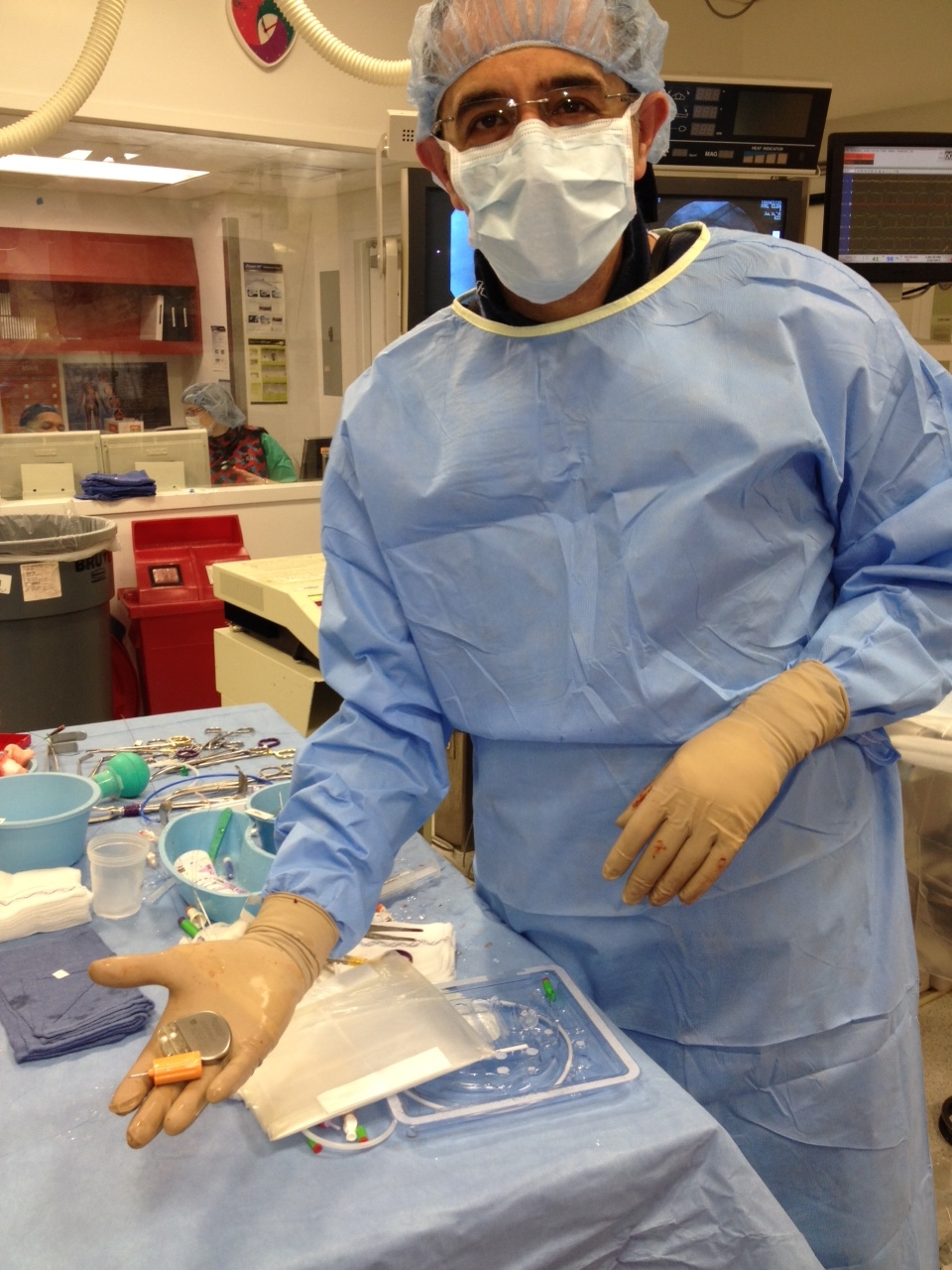

New York, NY (May 9, 2012) -- St. Luke’s and Roosevelt Hospitals is among the first hospitals in the U.S. and the first in the east coast to treat patients with an INGENIO™ pacemaker, manufactured by BostonScientific. Pacemakers are designed to treat bradycardia, a condition in which the heart beats too slowly -- usually less than 60 beats per minute -- depriving the body of sufficient oxygen.
“The INGENIO device enables physicians to treat pacemaker patients with an advanced and comprehensive set of therapies,” said Emad Aziz, DO, MB, C
HB, FACC, Attending Electrophysiologist, the Department of Medicine and Cardiology at St. Luke’s and Roosevelt Hospitals in New York “using the patient most accurate parameter of breathing; minute ventilation (MV), The INGENIO pacemaker’s MV sensor is easy to optimize and will provide needed therapy for patients with chronotropic incompetence to help them feel less fatigued during physical activity.”INGENIO pacemakers feature RightRate™ technology. RightRate utilizes Boston Scientific’s minute ventilation (MV) sensor and adds programming options that promote ease of use and time savings in-clinic. Boston Scientific’s MV sensor is the only sensor clinically proven to restore chronotropic competence. Chronotropic Incompetence (CI) is the inability of the heart to regulate its rate appropriately in response to physical activity, which may cause patients to feel tired or short of breath during daily activities such as walking or carrying groceries. CI affects up to 42 percent of pacemaker patients.
The INGENIO pacemaker will also have the capacity to transmit implantable cardiac device data from the device to physicians and other healthcare providers. Boston Scientifics' new LATITUDE NXT® Remote Patient Management system, currently under review by the FDA, will let physicians conduct remote follow-ups of these device patients to monitor specific device information and heart health status. The system will also detect clinical events between scheduled visits and send relevant data directly to a secure website, which can be accessed by physicians. This wireless technology will allow patients to transmit data to physicians from most locations in North America without the need for landline-based technology. Read More.
Several University Medical Practices Associates (UMPA) cardiologists also gave presentations, including Emad F. Aziz, DO, MB C HB, FACC; Farooq A. Chaudhry, MD, FACC, FASE; and Eyal Herzog, MD, FACC.Dr. Aziz spoke on the gap in healthcare management and the role of the Advanced Cardiac Admission Program (ACAP). Dr. Chaudhry discussed the role of echocardiography in identifying patients at risk for SCD and the role of CRT therapy for heart failure patients. And Dr. Herzog spoke about the use of a novel clinical pathway – called ESCAPE – (low Ejection fraction and Sudden Cardiac death Awareness and Prevention Eligibility) to prevent sudden cardiac arrest. The symposium also included a question and answer session. According to Dr. Aziz, one of the key presentation highlights was the finding that only about 20 percent of all patients eligible for implantable cardioverter defibrillator (ICD) therapy receive it. The rest are lost to follow-up or are not referred for evaluation for this treatment. Various myths about sudden cardiac death were also discussed during the event. Dr. Andrew Krahn’s lecture highlighted that the road is still in its beginning in identifying the genetics behind sudden cardiac death; “We only touched the peak of the iceberg when it comes to genetic predisposition and sudden cardiac death” said Dr. Krahn. Read More. Another SCD educational symposium is being planned for October, which is National Sudden Cardiac Arrest Awareness Month.
|
||||
The program included Dr. Janet Shapiro, director of the Intensive Care Unit, Dr. Jacqueline Holland-Tamis, Director of Interventional Fellowship and Dr. Eyal Herzog, spoke about women and heart disease, the utility of the hypothermia therapy after out of hospital cardiac arrest and voice of survivors, their families and first responders. It was great emotional and uplifting conference with an amazing honor for all the patients and their families. Read More.
|
||||
We concluded that in this real world prospective study contradicts the recent published data of ICD overuse and reveals the significant gap and underutilization of ICD among eligible patients’ |
||||

 On
Tuesday, April 24, over 100 healthcare professionals from St.
Luke’s and Roosevelt Hospitals attended an educational symposium
at St. Luke’s Hospital to promote sudden cardiac death (SCD)
awareness that was hosted by the ACAP Cardiac Research Group.
The event featured Andrew D. Krahn, MD, FACC, FHRS, President of
the Canadian Heart Rhythm Society, who spoke on the genetic
predictors related to this disorder.
On
Tuesday, April 24, over 100 healthcare professionals from St.
Luke’s and Roosevelt Hospitals attended an educational symposium
at St. Luke’s Hospital to promote sudden cardiac death (SCD)
awareness that was hosted by the ACAP Cardiac Research Group.
The event featured Andrew D. Krahn, MD, FACC, FHRS, President of
the Canadian Heart Rhythm Society, who spoke on the genetic
predictors related to this disorder. 
 The
ACAP program at St. Luke's and Roosevelt Hospitals hosted the
second Chilling in Manhattan Symposium "
The
ACAP program at St. Luke's and Roosevelt Hospitals hosted the
second Chilling in Manhattan Symposium "
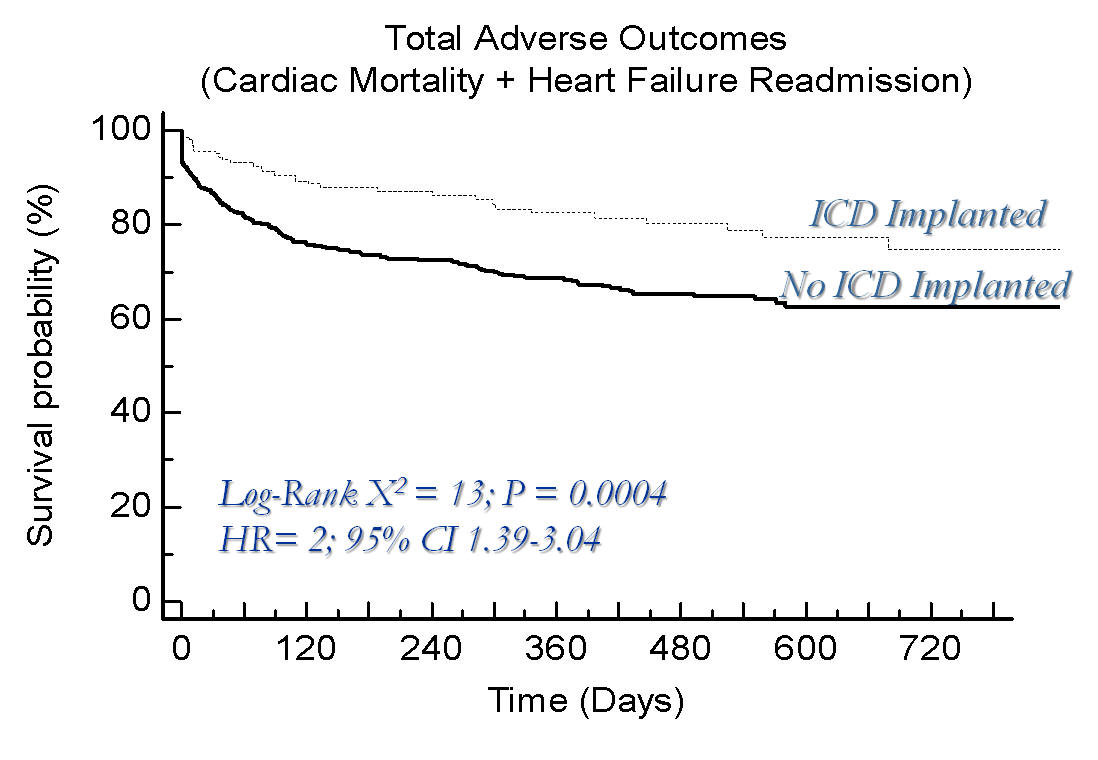
 The
ACAP program at St. Luke's and Roosevelt Hospitals presented
their latest research at the American College of Cardiology 61st
Annual scientific session in Chicago last month. The research
paper titled "A Major Gap Still Exists in Applying Published
Guidelines for primary Prevention of Sudden Cardiac Death and
Underutilization of Device Implantation; An ESCAPE Registry
Analysis" aimed to to evaluate the number of implanted devices
in a cohort of eligible patients according to the guidelines,
patient outcomes including all-cause mortality at 90 days and
heart failure readmissions at 30 days, and identifying any
differences among different race groups, sexes and Over-all
event rates at 24 month.
The
ACAP program at St. Luke's and Roosevelt Hospitals presented
their latest research at the American College of Cardiology 61st
Annual scientific session in Chicago last month. The research
paper titled "A Major Gap Still Exists in Applying Published
Guidelines for primary Prevention of Sudden Cardiac Death and
Underutilization of Device Implantation; An ESCAPE Registry
Analysis" aimed to to evaluate the number of implanted devices
in a cohort of eligible patients according to the guidelines,
patient outcomes including all-cause mortality at 90 days and
heart failure readmissions at 30 days, and identifying any
differences among different race groups, sexes and Over-all
event rates at 24 month.